Health & Safety: A Look Back, Gallop Ahead
By
John E. (Jack) Roberts
MHSAA Executive Director, 1986-2018
August 7, 2015
We are just completing year six of eight during which we have been addressing the four important health and safety issues that, for ease of conversation, we call the “Four Hs.”
During the 2009-10 and 2010-11 school years, our focus was on Health Histories. We made enhancements in the pre-participation physical examination form, stressing the student’s health history, which we believe was and is the essential first step to participant health and safety.
During the 2011-12 and 2012-13 school years, our focus was on Heads. We were an early adopter of removal-from-play and return-to-play protocols, and our preseason rules/risk management meetings for coaches included information on concussion prevention, recognition and aftercare.
Without leaving that behind, during the 2013-14 and 2014-15 school years, our focus was on Heat – acclimatization. We adopted a policy to manage heat and humidity – it is recommended for regular season and it’s a requirement for MHSAA tournaments. The rules/risk management meetings for coaches during these years focused on heat and humidity management.
At the mid-point of this two-year period, the MHSAA adopted policies to enhance acclimatization at early season practices and to reduce head contact at football practices all season long.
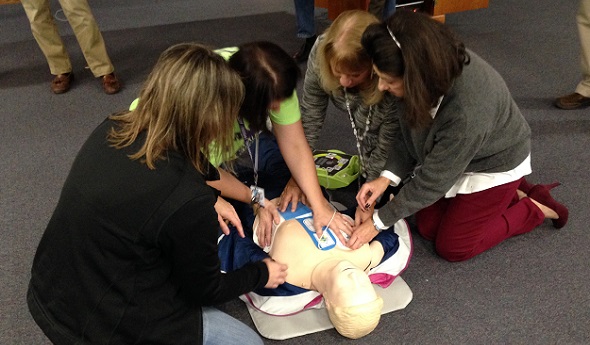
Without leaving any of the three previous health and safety “H’s” behind, during the 2015-16 and 2016-17 school years, our focus will be on Hearts – sudden cardiac arrest and sudden cardiac death.
Coinciding with this emphasis is the requirement that all high school level, varsity level head coaches be CPR certified starting this fall. Our emphasis will be on AEDs and emergency action plans – having them and rehearsing them.
On Feb. 10, bills were introduced into both the U.S. Senate and House of Representatives, together called the “Safe Play Act (see below),” which addressed three of the four health and safety “H’s” just described: Heat, Hearts and Heads.
For each of these topics, the federal legislation would mandate that the director of the Centers for Disease Control develop educational material and that each state disseminate that material.
For the heat and humidity management topic, the legislation states that schools will be required to adopt policies very much like the “MHSAA Model Policy to Manage Heat and Humidity” which the MHSAA adopted in March of 2013.
For both the heart and heat topics, schools will be required to have and to practice emergency action plans like we have been promoting in the past and distributed to schools this summer.
For the head section, the legislation would amend Title IX of the 1972 Education Amendments and eliminate federal funding to states and schools which fail to educate their constituents or fail to support students who are recovering from concussions. This support would require multi-disciplinary concussion management teams that would include medical personnel, parents and others to provide academic accommodations for students recovering from concussions that are similar to the accommodations that are already required of schools for students with disabilities or handicaps.
This legislation would require return-to-play protocols similar to what we have in Michigan, and the legislation would also require reporting and recordkeeping that is beyond what occurs in most places.
This proposed federal legislation demonstrates two things. First, that we have been on target in Michigan with our four Hs – it’s like they read our playbook of priorities before drafting this federal legislation.
This proposed federal legislation also demonstrates that we still have some work to do.
And what will the following two years – 2017-18 and 2018-19 – bring? Here are some aspirations – some predictions, but not quite promises – of where we will be.
First, we will have circled back to the first “H” – Health Histories – and be well on our way to universal use of paperless pre-participation physical examination forms and records.
Second, we will have made the immediate reporting and permanent recordkeeping of all head injury events routine business in Michigan school sports, for both practices and contests, in all sports and at all levels.
Third, we will have added objectivity and backbone to removal from play decisions for suspected concussions at both practices and events where medical personnel are not present; and we could be a part of pioneering “telemedicine” technology to make trained medical personnel available at every venue for every sport where it is missing today.
Fourth, we will have provided a safety net for families who are unable to afford no-deductible, no exclusion concussion care insurance that insists upon and pays for complete recovery from head injury symptoms before return to activity is permitted.
We should be able to do this, and more, without judicial threat or legislative mandate. We won’t wait for others to set the standards or appropriate the funds, but be there to welcome the requirements and resources when they finally arrive.
Safe Play Act — H.R.829
114th Congress (2015-2016) Introduced in House (02/10/2015)
Supporting Athletes, Families and Educators to Protect the Lives of Athletic Youth Act or the SAFE PLAY Act
Amends the Public Health Service Act to require the Centers for Disease Control and Prevention (CDC) to develop public education and awareness materials and resources concerning cardiac health, including:
- information to increase education and awareness of high risk cardiac conditions and genetic heart rhythm abnormalities that may cause sudden cardiac arrest in children, adolescents, and young adults;
- sudden cardiac arrest and cardiomyopathy risk assessment worksheets to increase awareness of warning signs of, and increase the likelihood of early detection and treatment of, life-threatening cardiac conditions;
- training materials for emergency interventions and use of life-saving emergency equipment; and
- recommendations for how schools, childcare centers, and local youth athletic organizations can develop and implement cardiac emergency response plans.
Requires the CDC to: (1) provide for dissemination of such information to school personnel, coaches, and families; and (2) develop data collection methods to determine the degree to which such persons have an understanding of cardiac issues.
Directs the Department of Health and Human Services to award grants to enable eligible local educational agencies (LEAs) and schools served by such LEAs to purchase AEDs and implement nationally recognized CPR and AED training courses.
Amends the Elementary and Secondary Education Act of 1965 to require a state, as a condition of receiving funds under such Act, to certify that it requires: (1) LEAs to implement a standard plan for concussion safety and management for public schools; (2) public schools to post information on the symptoms of, the risks posed by, and the actions a student should take in response to, a concussion; (3) public school personnel who suspect a student has sustained a concussion in a school-sponsored activity to notify the parents and prohibit the student from participating in such activity until they receive a written release from a health care professional; and (4) a public school's concussion management team to ensure that a student who has sustained a concussion is receiving appropriate academic supports.
Directs the National Oceanic and Atmospheric Administration to develop public education and awareness materials and resources to be disseminated to schools regarding risks from exposure to excessive heat and humidity and recommendations for how to avoid heat-related illness. Requires public schools to develop excessive heat action plans for school-sponsored athletic activities.
Requires the CDC to develop guidelines for the development of emergency action plans for youth athletics.
Authorizes the Food and Drug Administration to develop information about the ingredients used in energy drinks and their potential side effects, and recommend guidelines for the safe use of such drinks by youth, for dissemination to public schools.
Requires the CDC to: (1) expand, intensify, and coordinate its activities regarding cardiac conditions, concussions, and heat-related illnesses among youth athletes; and (2) report on fatalities and catastrophic injuries among youths participating in athletic activities.
'Retired' Periard Still Finding Ways to Serve Suttons Bay
By
Tom Spencer
Special for MHSAA.com
May 28, 2021
When Doug Periard retired in August, some thought he had done it all as a teacher, coach, mentor and athletic director for Suttons Bay Schools.
 Retirement has proven many wrong.
Retirement has proven many wrong.
He did intend to stay on as the baseball coach at least thru the 2022 season. He also thought he’d help out some with the bus driver shortage using the CDL (Commercial Drivers License) he’d recently obtained. Substitute teaching sounded good to him too.
So he came back in October. He immediately took on an emergency assignment, coaching the school’s 8-player football team to a win over Manistee Catholic Central. He also drove the bus to the game.
“Doug is that kind of guy ... when there is a need to filled, Doug will fill it for you,” said Andy Melius, principal at Suttons Bay. “The community means a lot to him, and the school means a lot to him. He bleeds red and white.”
Also since returning, he’s served as a K-1 gym teacher, filled in at the school’s front desk and headed up the district’s COVID-19 testing as the Quarantine Officer.
On Tuesday, Periard will coach baseball after driving the bus transporting the Norsemen to Buckley to begin postseason play. It’s no different than what he’s been doing all spring.
However, some questioned if Periard could handle bus driving and coaching on the same day.
 “It’s been interesting,” Periard said with a little laugh. “I was a champion at taking a nap (on the bus as coach).
“It’s been interesting,” Periard said with a little laugh. “I was a champion at taking a nap (on the bus as coach).
“I would be asleep before we got to the split in the road and wake up when we got there,” he continued. “So, there was some real skeptics out there wondering if I’d be able to both drive and coach when I got there.”
Periard has hopes of hitting the 400-win mark before giving up baseball. He’s compiled a 379-280-18 record since taking over the Norseman baseball program on a “temporary” basis in 1998. It was supposed to be only until another coach was found. He had coached the JV squad the year prior.
And, there’s something else about Periard very few people know. Someone who does is Christine Mikesell, Suttons Bay’s assistant athletic director. Mikesell’s five boys at one time or another played sports coached by Periard.
“Every kid is important to Doug,” noted Mikesell, who is stepping down in June. “He really has a big heart for those that are struggling, and he makes a pathway for a kid to achieve if they take it.
“He is one of those kind of guys you want on your side because he is a team player ... a real team player when it comes to the school and athletics and coaching.”
Mikesell has seen him help lots of high schoolers who end up graduating perhaps without knowing how much help Periard provided. He often made sure kids had a white dress shirt so no one was left out on the school’s game day dress-up tradition. He’s also paid for lunches and arranged transportation for students coming from hard-life circumstances.
“I have seen him go well out of his way,” said Mikesell. “I know a lot of it is his own pocket.
“He has eyes, and he watches,” she continued. “He finds the one that is struggling, and he goes and brings them as part of the team.”
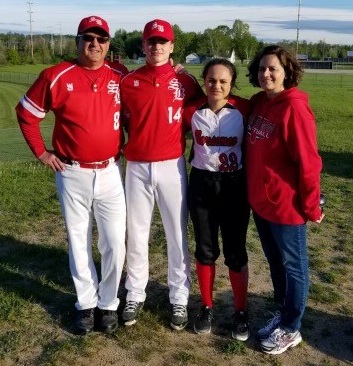
Periard became AD in 2008, a year he will never forget. It was marked by the stock market crash and he, along with his wife Anne, was dealing with his daughter Grace’s new diabetes diagnosis. The economic circumstances also threatened his continued employment as a teacher.
The job loss did not materialize. Grace is now in college. And, she was the 2020 recipient of the Suttons Bay High School Berserker Award presented to Norse athletes who have competed in three sports every year of high school.
The award was created several years back by Periard. Now he hopes his son Hugh, a junior pitcher and three-sport athlete, will follow his sister’s footsteps and be similarly recognized next spring.
“I stole the (Berserker) idea from my little brother who was the AD at Birch Run,” he admitted. “I am proud to have gotten the thing rolling.
“I think playing three sports is vital to a small school and development of young people.”
Periard’s legacy also will include strong co-op developments, including the establishment of NorthBay, and keeping a great football tradition alive while the school struggled with declining enrollment. The co-ops are established for all sports with Northport and include Leelanau St. Mary’s in boys and girls track & field and soccer.
 Periard guided the Norsemen’s move to 8-player football in 2017. The previous season, Suttons Bay had to forfeit the majority of its games because it did not have enough players to compete in 11-player.
Periard guided the Norsemen’s move to 8-player football in 2017. The previous season, Suttons Bay had to forfeit the majority of its games because it did not have enough players to compete in 11-player.
Mikesell’s son Baylor was one of seniors who missed out as part of that 2016 team. Another son, Lucas, was a star player in the school’s run to back-to-back 8-player Division 2 runner-up finishes the last two seasons.
“My son lost his senior year because we were still 11-man, and we couldn’t field a team,” she said. “Doug is a problem solver and comes up with solutions outside the box.
“He did tons of research on it to get us in a place (where) we could participate in football because he saw that the risk of losing football here at the school, what a damaging thing it would be.”
Periard is most proud, however, of the behavior of the student body during athletic contests. His game management included a “bristle” – a knowing look – passed on from his grandfather to his mother and ultimately to he and his brothers.
With his simple bristle he was able to instantly, and non-verbally, communicate to the students they’d better stop what they’re doing.
“They bought into my stern look when they were in any way at all not cheering for their team,” he said. “They knew they should be cheering for their teams and not being disparaging against their opponent, and only treating opponents with class.”
 Tom Spencer is a longtime MHSAA-registered basketball and soccer official, and former softball and baseball official, and he also has coached in the northern Lower Peninsula area. He previously has written for the Saginaw News, Bay County Sports Page and Midland Daily News. He can be reached at [email protected] with story ideas for Manistee, Wexford, Missaukee, Roscommon, Ogemaw, Iosco, Alcona, Oscoda, Crawford, Kalkaska, Grand Traverse, Benzie, Leelanau, Antrim, Otsego, Montmorency, Alpena, Presque Isle, Cheboygan, Charlevoix and Emmet counties.
Tom Spencer is a longtime MHSAA-registered basketball and soccer official, and former softball and baseball official, and he also has coached in the northern Lower Peninsula area. He previously has written for the Saginaw News, Bay County Sports Page and Midland Daily News. He can be reached at [email protected] with story ideas for Manistee, Wexford, Missaukee, Roscommon, Ogemaw, Iosco, Alcona, Oscoda, Crawford, Kalkaska, Grand Traverse, Benzie, Leelanau, Antrim, Otsego, Montmorency, Alpena, Presque Isle, Cheboygan, Charlevoix and Emmet counties.
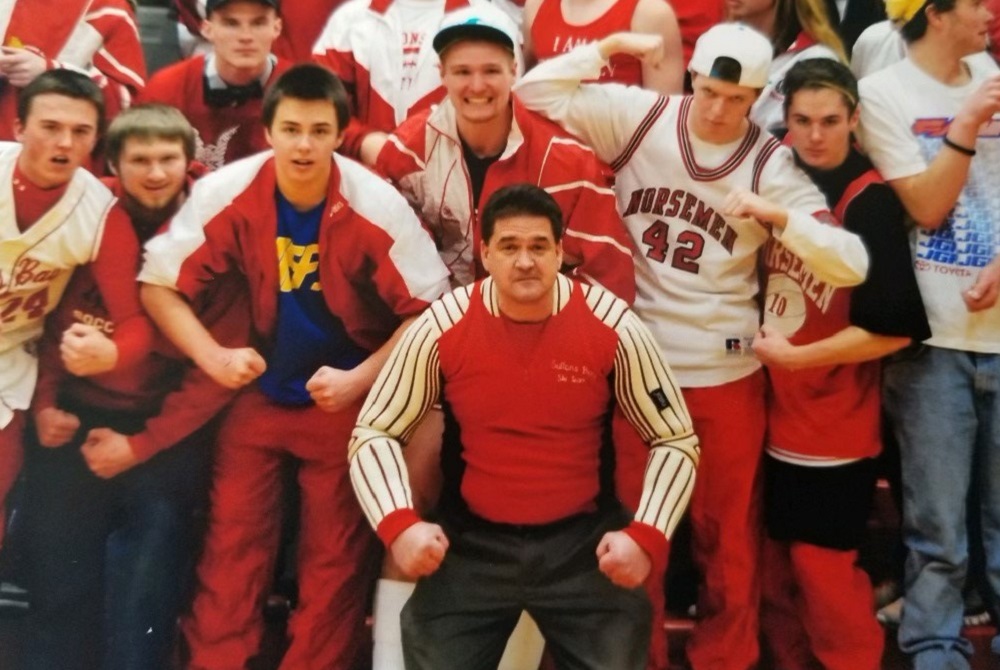
PHOTOS: (Top) Doug Periard enjoys a moment surrounded by enthusiastic Suttons Bay student fans during his tenure. (Middle) Periard, also the baseball coach, with son Hugh, daughter Grace and wife Anne a few years ago. (Below) Even in retirement, Periard remains a mainstay in Suttons Bay. (Top and middle photos courtesy of Doug Periard; bottom photo by Tom Spencer.)

